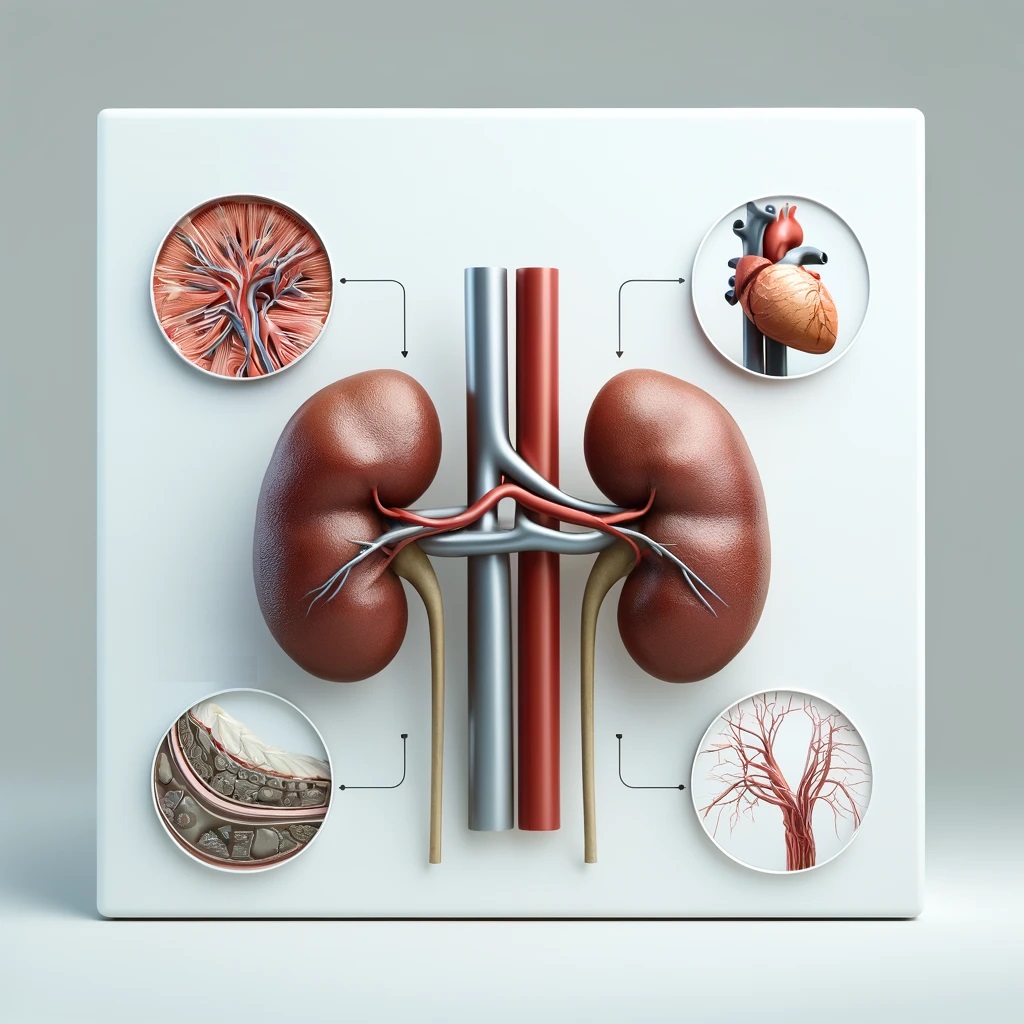
Chronic Kidney Disease (CKD) is frequently complicated by mineral metabolism disorders, which significantly contribute to the increased cardiovascular morbidity and mortality observed in this population. These disorders, including hyperphosphatemia, hyperparathyroidism, and vitamin D deficiency, lead to vascular calcification, arterial stiffness, and cardiovascular events.
Pathophysiology of Mineral Metabolism Disorders in CKD
In CKD, the kidneys’ ability to maintain normal mineral metabolism is impaired, leading to several interconnected disturbances:
- Hyperphosphatemia: As kidney function declines, phosphate excretion is reduced, resulting in elevated serum phosphate levels. Hyperphosphatemia directly stimulates parathyroid hormone (PTH) secretion and contributes to secondary hyperparathyroidism. Excess phosphate binds to calcium, forming calcium-phosphate complexes that deposit in vascular tissues, leading to calcification and arterial stiffness.
- Secondary Hyperparathyroidism: Reduced renal function impairs the production of active vitamin D (calcitriol), leading to hypocalcemia. In response, the parathyroid glands secrete more PTH to maintain calcium homeostasis. Chronic elevation of PTH promotes bone resorption and increases serum calcium levels, further contributing to vascular calcification.
- Vitamin D Deficiency: The kidneys are responsible for converting inactive vitamin D to its active form, calcitriol. In CKD, reduced conversion leads to vitamin D deficiency, exacerbating hypocalcemia and secondary hyperparathyroidism. Vitamin D deficiency also directly impacts cardiovascular health by promoting inflammation, endothelial dysfunction, and left ventricular hypertrophy.
- Fibroblast Growth Factor 23 (FGF23): FGF23 levels rise in response to hyperphosphatemia and reduced calcitriol production. FGF23 helps maintain phosphate balance by increasing renal phosphate excretion and inhibiting calcitriol synthesis. However, elevated FGF23 is associated with left ventricular hypertrophy, increased arterial stiffness, and higher cardiovascular mortality in CKD patients.
Impact on Cardiovascular Health
Mineral metabolism disorders in CKD significantly impact cardiovascular health through several mechanisms:
- Vascular Calcification: The deposition of calcium-phosphate complexes in the vascular walls leads to arterial stiffness and reduced elasticity. This calcification increases systolic blood pressure and pulse pressure, contributing to left ventricular hypertrophy and heart failure.
- Endothelial Dysfunction: Hyperphosphatemia and secondary hyperparathyroidism promote endothelial dysfunction, characterized by reduced nitric oxide availability and increased oxidative stress. Endothelial dysfunction impairs vascular relaxation and promotes atherosclerosis.
- Inflammation and Oxidative Stress: Mineral metabolism disorders contribute to a pro-inflammatory state and oxidative stress, both of which are implicated in the pathogenesis of cardiovascular disease. Elevated phosphate levels and PTH stimulate inflammatory cytokine production, exacerbating cardiovascular damage.
- Left Ventricular Hypertrophy: Elevated FGF23 and secondary hyperparathyroidism are associated with left ventricular hypertrophy. This structural change in the heart increases the risk of heart failure and sudden cardiac death.
- Increased Cardiovascular Events: CKD patients with mineral metabolism disorders have a higher incidence of cardiovascular events such as myocardial infarction, stroke, and peripheral artery disease. These events significantly contribute to the high cardiovascular mortality in CKD.
Management Strategies
Effective management of mineral metabolism disorders in CKD is crucial to reducing cardiovascular risk. Key strategies include:
- Phosphate Binders: Phosphate binders are used to reduce intestinal phosphate absorption and control serum phosphate levels. Calcium-based binders (e.g., calcium acetate) and non-calcium-based binders (e.g., sevelamer, lanthanum carbonate) are commonly used. The choice of binder depends on serum calcium levels and the presence of vascular calcification.
- Vitamin D Supplementation: Active vitamin D analogues (e.g., calcitriol, paricalcitol) are used to treat vitamin D deficiency and secondary hyperparathyroidism. These agents help reduce PTH levels, improve calcium and phosphate balance, and have direct beneficial effects on cardiovascular health.
- Calcimimetics: Calcimimetics (e.g., cinacalcet) are used to control secondary hyperparathyroidism by increasing the sensitivity of the parathyroid gland to calcium. This reduces PTH secretion and helps manage serum calcium and phosphate levels, thereby reducing the risk of vascular calcification.
- Dietary Modifications: Dietary phosphate restriction is essential to manage hyperphosphatemia. Patients are advised to limit the intake of phosphate-rich foods, particularly processed foods and additives. Adequate dietary calcium intake should also be ensured to avoid hypocalcemia.
- Magnesium Supplementation: Emerging evidence suggests that magnesium supplementation may help inhibit vascular calcification by reducing calcium-phosphate precipitation and VSMC osteogenic differentiation. Magnesium supplements are being explored as a potential therapeutic option.
- Monitoring and Adjustment: Regular monitoring of serum calcium, phosphate, PTH, and vitamin D levels is crucial to guide therapy and adjust treatment plans. This helps maintain optimal mineral balance and minimize cardiovascular risk.
Conclusion
Mineral metabolism disorders in CKD, including hyperphosphatemia, secondary hyperparathyroidism, vitamin D deficiency, and elevated FGF23, significantly contribute to cardiovascular morbidity and mortality. These disorders promote vascular calcification, endothelial dysfunction, inflammation, oxidative stress, and left ventricular hypertrophy, all of which increase the risk of cardiovascular events.
Effective management requires a comprehensive approach that includes phosphate binders, vitamin D supplementation, calcimimetics, dietary modifications, and magnesium supplementation.
Quiz
Please note that our articles are not intended to guide personal health decisions.
This content has been curated by Renes Care. Unauthorized use or reproduction is prohibited.
© Renes Care. All rights reserved.
